The more than 27,000 seniors in publicly funded residential care in B.C. need more care hours, more freedom and more social interaction, says a report from B.C.’s seniors watchdog.
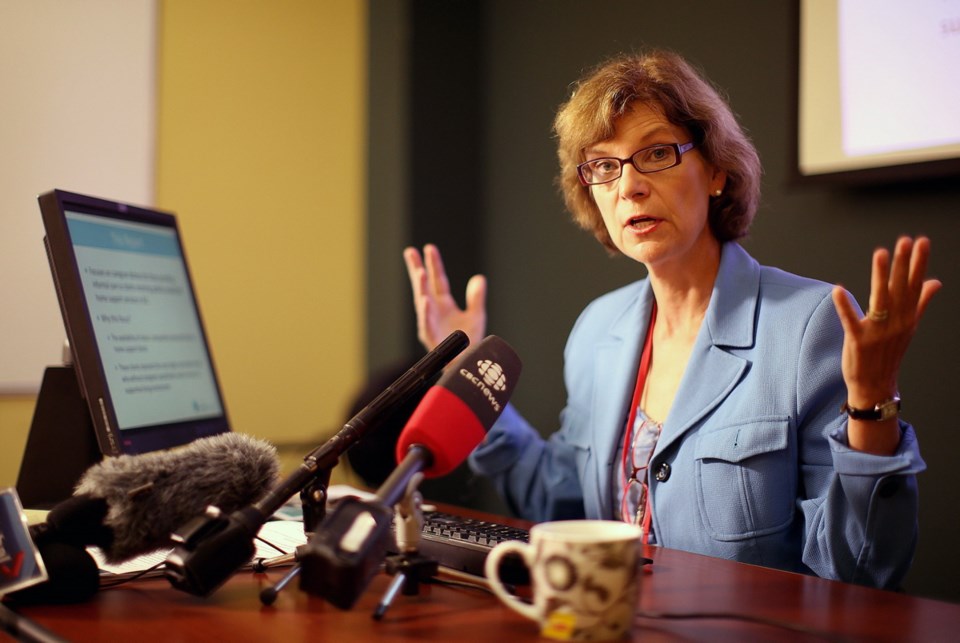
Almost 10,000 seniors in 292 publicly funded care homes were surveyed for the report, which was released Friday by seniors advocate Isobel Mackenzie.
The results show “staffing levels are a major concern for residents and their families,” Mackenzie said. “Consistent feedback is that there simply are not enough staff to ensure residents’ needs are taken care of when they need to be.”
Staffing also hampers flexibility in things such as bathing and eating times, social interactions and engagement in leisure activities — the main complaints of survey respondents.
Sixty-two per cent of residents said they do not get to bathe or shower as often as they want, “with a full 50 per cent saying it rarely or never happens as often as they want,” the report said. One in four residents said they only sometimes, rarely or never get help to the toilet when they need it.
“If I had to sum up what the 22,000 voices, the 10,000 residents, 10,000 family members are telling, it is we need more staff,” Mackenzie said. “We know in B.C. that over 80 per cent of our facilities are not staffed at the recommended level.”
Health Minister Adrian Dix said he has been mandated by Premier John Horgan to increase staffing levels to ensure seniors in B.C.’s public and private residential care facilities receive 3.36 hours of individual care daily.
“Certainly, there’s a staffing question,” he said. “We need to promote opportunities in care for people to live to the fullest extent of their freedom, which is what we all want to do in the course of our lives. At the heart of that is the fact that care homes are currently understaffed based on provincial guidelines.”
In the weeks before the May provincial election, the then-governing B.C. Liberals announced a four-year, $500-million care plan to meet the 3.36 hour daily-care target.
The plan called for 1,500 people to be hired, including health-care assistants, nurses, occupational therapists and physiotherapists.
Hospital Employees’ Union spokeswoman Jennifer Whiteside said the provincial government needs to move quickly to meet those commitments.
“There is a profound staffing crisis in residential long-term care,” she said. Staff are so rushed they say they can only perform the most basic and immediate tasks “and there isn’t time for anything beyond that.”
The union represents 49,000 health-care workers including about 20,000 who work in residential care facilities across the province.
Mackenzie said the stories and feedback paint a picture of a diverse group of men and women “who, through circumstances beyond their control, have found themselves living with folks many of them don’t really know; eating food that some like more than others; waiting for help that is sometimes too long in coming; and lacking the freedom to go and do what they want when they want.”
Still, most describe themselves as happy and would recommend that others come and live with them.
The survey showed 88 per cent of residents feel safe in their care home, 86 per cent say staff treat them with respect and 93 per cent think the care home is clean.
However, “there is an overall sense of loneliness that many, although not all, residents express,” Mackenzie said.
The report found almost 46 per cent of residents said there is no one living in the facility they consider a close friend and 45 per cent say there is no one to do things with, she said.
The results of the survey do not show a residential care system that is failing overall, but it does show there are major issues, she said, mostly with respect to staffing levels.
“There simply are not enough staff to ensure residents’ needs are taken care of when they need to be.”
— With a file from The Canadian Press
Recommendations
• Increase staffing in care facilities.
• Increase flexibility around when and how care is delivered.
• Increase activities for weekends and evenings and create more meaningful experiences overall.
• Provide better medical care either through general practitioners and/or explore further increasing the role of nurse practitioners.
• Examine opportunities to improve the meal time experience, particularly flexibility with meal times.
• Provide ongoing education for all care staff on the importance of resident emotional well-being.
• Foster greater engagement with family members
— Source: Every Voice Counts: Office of Seniors Advocate Residential Care Survey Provincial Results