Island Health is trying to address the overdose crisis in Victoria with a new injectable treatment for chronic opioid addiction.
Injectable Opioid Agonist Treatment, referred to as iOAT, will be offered to residents of Johnson Street Community, a supportive housing facility downtown with capacity for 147 residents. The injectable treatment is available for residents who have not benefited from orally administered treatment options, which include methadone, suboxone, and kadian.
Twenty-three people died from overdoses in Victoria in the first five months of 2019, placing the city third behind Vancouver and Surrey in total number of overdose deaths in the province.
In 2017 and 2018, more than 90 people died of an overdose in Victoria, and about 1,500 in the province both years.
PHS Community Services Society, which provides low-barrier housing and services for marginalized people, will provide the treatment under a contract with Island Health.
Kelly Reid, director of mental health and substance-use services for Island Health, said the new treatment is coming to Victoria in response to the overdose crisis that has affected all communities in B.C. and across the country.
“The iOAT is an evidence-based service that helps individuals to significantly reduce the risk of opioid overdose death and to stabilize their use of substances,” Reid said.
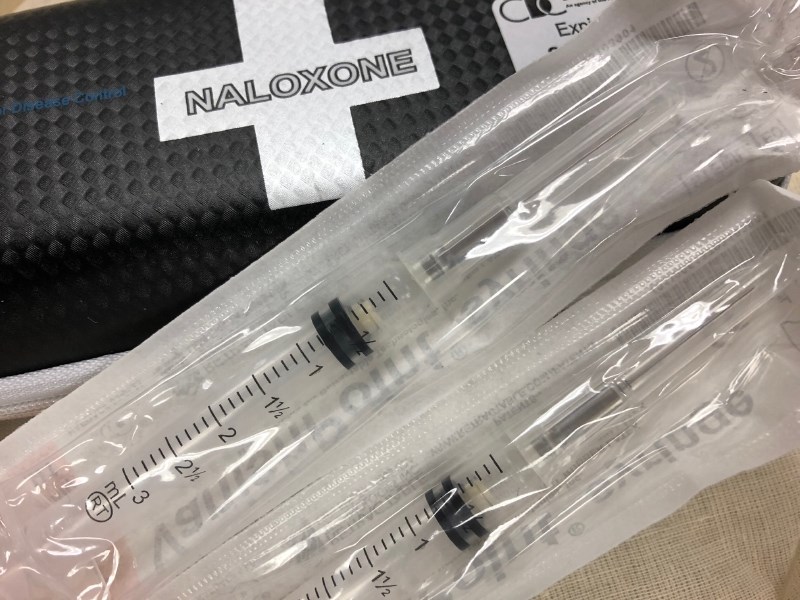
The treatment of pharmaceutical-grade, prescription opioid will be provided twice daily. Doses are drawn up by a nurse who can administer the treatment, or patients can self-administer under observation. The treatment, like oral options, is meant to replace the use of illicit opioids.
“When someone has ongoing illicit opiate use, you want to move them off of that illicit market, because they’re funding organized crime,” said Christy Sutherland, medical director at the PHS Community Services Society. “They’re having to commit crimes to get those drugs. And then when they buy it, they don’t know what they’re getting. And this is why we’re having these overdoses because people are using carfentanyl or fentanyl when they’re just intending to use heroin.”
Sutherland said oral opioid treatment options work only for about 50 per cent of people living with chronic use. For those who find it doesn’t work, they might still experience cravings, use illicit drugs and be at risk of an overdose.
“We’ve known for decades that these oral options don’t work for everyone,” Sutherland said. “So for this population who has ongoing IV drug use, perhaps ongoing overdoses and is really suffering and vulnerable and at high risk of death — despite really good access to oral options — what they need is the injectable option.”
The injectable treatment will be offered to six patients to start, and grow to a capacity of 20 patients.
The Ministry of Health is providing about $500,000 to $900,000 in annual funding for the treatment.
Sutherland said while some might think it’s counterintuitive to provide opioids to patients as treatment, it’s a cost-effective way to treat chronic use.
“It actually saves money. It decreases death and decreases overdoses. It decreases how much money is spent in the illicit market,” she said. “It decreases public disorder. We don’t want people breaking into cars, or stealing, or having to do panhandling.”
PHS has offered the injectable treatment in Vancouver since 2016. Sutherland said it has been a joy to see how patients’ quality of life improves with the treatment.
“They stopped committing crime. They stopped going to jail. Often they reconnect with their family, and they get work. They just look like a million bucks. It’s just really a wonderful thing to do as a doctor to be able to provide the service,” she said.