Emergency-medicine specialists at a busy West Shore clinic want to host a physician-assistant pilot program, promising to increase the number of patients treated at a lower cost while attaching more patients to doctors.
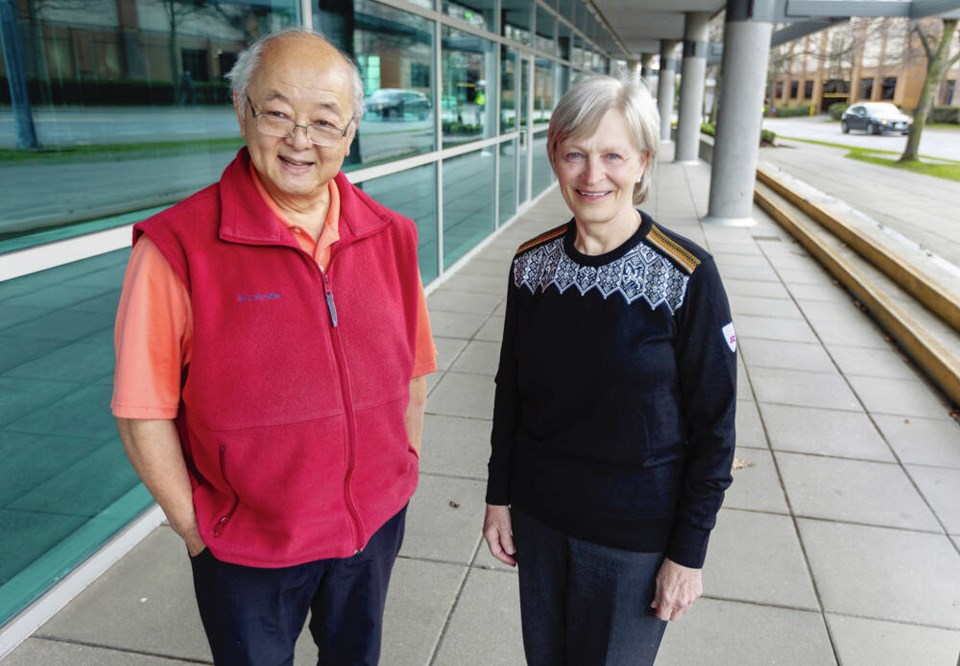
Dr. Charles Sun and Dr. Jane Moran said they could increase by 50 per cent the number of patients they see, and cut the number of patients without a doctor in Langford and Juan de Fuca to 1,600 from 8,000.
“We need to bring in everybody that’s available and capable to provide assistance,” said Sun, who retired in 2016 but returned to practice in 2018 to work at the West Shore Urgent and Primary Care Centre.
The two are proposing three physician assistants, who would be licensed to practice with physician supervision, for the West Shore UPCC. That would allow for one physician assistant working with the physician on duty, seven days a week.
The physician assistant’s presence would allow the physician to just see the more complex patients, they said.
In the beginning, each physician assistant would see a minimum of 10 patients per shift, said Sun. Within three to six months, the number of patients seen by the physician assistant could increase to 15 or more per shift, they said.
The number of patients a physician can typically see a day ranges from 12 to 25, depending on the complexity of the patients’ needs.
Physician assistants — who have so far not been licensed to practise in B.C. — would be roughly 30 to 40 per cent cheaper for the health-care system than physicians, Sun and Moran said, yet the patient receives “physician-quality care.”
The West Shore doctors say each physician assistant could extend the physician’s reach in a family practice by 1,000 patients, increasing the number of patients seen each day.
Based on an average physician assistant annual compensation of $80,000 to $135,000, the pilot would potentially cost the province $240,000 to $405,000 for a year’s wages — or half that for a six-month pilot.
All care data would be collected, analyzed and reported to evaluate the program’s success, the doctors said.
“The concept has already been proven,” said Sun, “we just need implementation of the profession given the medical crisis.”
The West Shore UPCC has four physicians who have previously worked with physician assistants, who are licensed to practise in several countries, including the United States, as well as in Ontario, Manitoba, Alberta, New Brunswick and Nova Scotia.
Newfoundland and Saskatchewan are working with the Canadian Association of Physician Assistants to introduce physician assistants in those provinces, said Lisa Stewart, association director for B.C.
Physician assistants are educated under the same medical model as doctors through a 24-month graduate program, making them a more immediate solution to the health-care crisis, Sun said.
Training is available at three sites in Canada: the University of Manitoba, the University of Toronto and a satellite site at McMaster University in Hamilton, Ont., all of which are increasing enrolment.
Three more university programs are in development in Ontario, Saskatchewan and Alberta, Stewart said.
Canadian Forces Medical Services School at CFB Borden also provided the training but that has now ended.
Stewart suggests a physician-assistant training program could be created at the University of Victoria, while Sun and Moran suggest the Justice Institute of B.C., where paramedics are trained.
Almost 1,000 physician assistants are already trained in Canada, according to the Canadian Association of Physician Assistants.
Sun began his career in emergency medicine in 1973 and said that for 35 years, he has been “championing the cause of PAs.”
Working from 2000 to 2012 as a Victoria ER physician and medical director for B.C. Emergency Health Services, he headed a group of five physicians at Royal Jubilee Hospital and Victoria General Hospital updating the training of Canadian Forces physician assistants going on tours of duty in Somalia and Afghanistan.
The pilot project was “overwhelmingly successful,” he said.
Physician assistants can prescribe most medicines, conduct patient interviews, provide physical exams, perform diagnostic tests, order and read tests, and make referrals under a physician’s guidance.
They can typically tend to about 80 per cent of the daily patient load for family doctors, said Sun.
Moran, a UBC associate clinical professor in the Faculty of Medicine, likens a physician assistant to a chief resident who has trained with a physician for five years and is ready to work independently. “A physician assistant is a chief resident who never leaves your practice,” said Moran.
Moran said it makes no sense for B.C. Health Minister Adrian Dix to tout team-based care and reject physician assistants.
Some have said nurse practitioners could play the same role, but the difference, said Moran, is that a physician assistant has the full scope of the supervising physician.
Moran points to members of ambulance infant transport teams who are trained in specialized care to transport critically ill newborns and pediatric patients.
Just as physician assistants work in collaboration with a physician, infant transport team members are directed by B.C. Children’s Hospital neonatologists and intensivists.
Moran maintains physician assistants are “best suited” to rural areas, given that they can independently interpret X-rays, set a fracture, put a cast on, sew a laceration, intubate a patient, and remove foreign bodies from ears and noses.
Troy Clifford, president of the Ambulance Paramedics and Dispatchers of B.C., said he’s in favour of physician assistants in B.C., which he said would help expand physicians’ scope, particularly in rural, remote and Indigenous communities.
Trevor Stone, 60, of Comox was a medic in the Canadian Forces in Victoria when he took a 26-month physician-assistant program through the Forces, which uses them on its ships, submarines and bases.
When Stone retired from the Forces in 2006, he was forced to work in Winnipeg because B.C. does not permit physician assistants to practice in the province. In Winnipeg, he assisted surgeons in reconstructive plastic surgery. Many physician assistants want to work in B.C., with the only roadblock being the Health Ministry, he said. “It’s frustrating.”
Many times during his decades of advocating for physician assistants, Sun has been told approval was just around the corner only to have his hopes dashed.
In March 2022, on behalf of Dix, physician services executive director Kevin Brown wrote “there are no identified care gaps that can be specifically filled by the PAs.”
Sun said the gaps are “everywhere,” which is why, after five decades, he’s still practising at West Shore’s UPCC. “I am by far not the only physician who has continued to practice or come out of retirement to serve our needy community.”
In the past two years, more than 50 per cent of West Shore UPCC physicians have left. On the days when there’s not enough physician coverage, the UPCC must close, which is “a very alarming circumstance” for both patients and staff, said Sun. Also, of those lining up outside the centre each morning, 25 to 30 per cent have a family doctor and just can’t get an appointment to see them, said Sun.
Dix has said he’s open to looking at the issue, but that the province has focused its investments on nurse practitioners and associate physicians, doctors trained outside Canada and not yet licensed to practice independently here.
The Doctors of B.C., representing 14,000 physicians, has recommended physician assistants since 2006. The following year, the Society of General Practitioners of B.C. said 150,000 people did not have a family doctor in B.C. Now, the number is estimated at about one million people.
Dr. Joshua Greggain, president of Doctors of B.C., said if anyone is blocking physician assistants, it’s not the Doctors of B.C. or the College of Physician and Surgeons.
“I think the bigger conversation is around where they fit, and ultimately then who funds them?” said Greggain. “But I think the more help the better.”
Greggain said there’s “lots of appetite” for having having physician assistants in rural areas across the province in all five health authorities. “We need to start somewhere and I think acknowledging the challenges in the North Island is a great opportunity.”
>>> To comment on this article, write a letter to the editor: [email protected]