Camosun College has developed another device to help in the fight against COVID-19: a portable “oven” that uses ultraviolet light to sterilize N95 masks so they can be reused by health-care workers.
The Camosun Innovates centre at the Interurban campus previously launched a new medical-grade face-shield design. To date, thousands of the face shields have been produced by the private sector.
Its latest prototype, called UVen, can be set up in hospitals, walk-in clinics, doctors’ offices and fire halls, and can be easily moved to another location if needed.
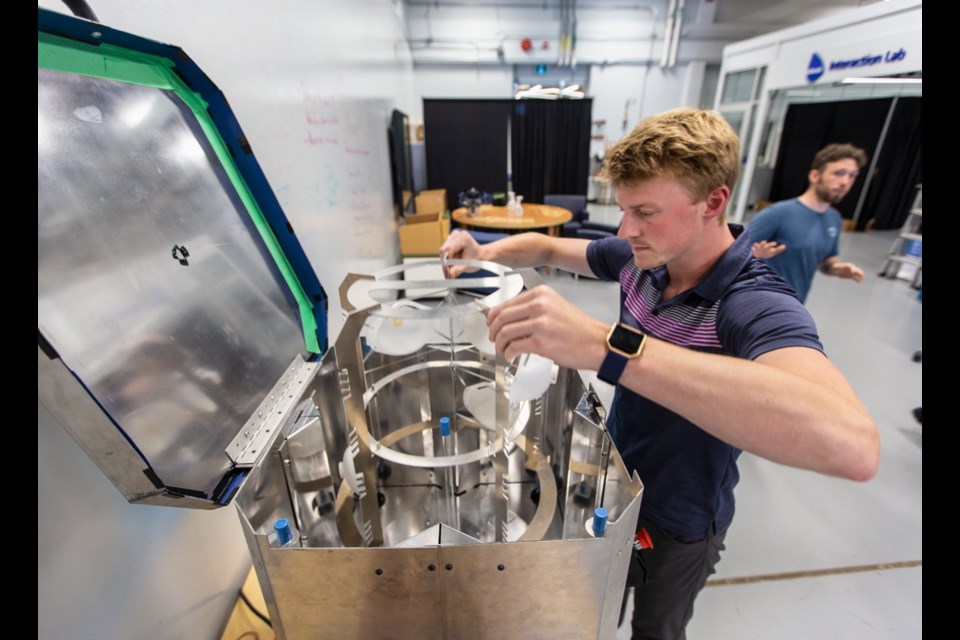
About the size of a mini-fridge, it weighs less than 20 kilograms. Masks are placed on an internal carousel that revolves to ensure the entire mask is decontaminated in 30 minutes, said Richard Gale, director of Camosun Innovates, a research and development centre with manufacturing capabilities.
An N95 mask can typically be cleaned four or more times, depending on its condition, Gale said, and the UVen can sterilize 10 masks at a time.
He is hoping that with a “few more tweaks,” it will be possible to clean 15 masks at once in a 15-minute time frame.
The oven was developed because Island Health was looking at ways to extend the life of personal protective equipment through local decontamination.
As possibilities were considered, relying on UV light was appealing because it is efficient, leaves no residue, is environmentally sound, and uses materials commonly available, such as sheet metal, aluminum and regular UV light bulbs, Gale said. The UVen runs on standard voltage.
Gale anticipates that the first five UVens will be used by Island Health within weeks. He expects that as models are refined, the cost for one would be about $500 to $600.
Victoria Schmid, vice-president of pandemic planning with Island Health, said in a statement that the UVen project allows the health authority to test how each og its respirator models reacts to ultraviolet sterilization. “Should the supply chain ever get compromised, we can make data-informed decisions to protect our staff and patients.”
Personal protective equipment such as N95 masks has been in short supply.
N95 masks are supposed to be used only once unless they can be decontaminated.
Camosun Innovates “can do a lot of things quickly and creatively” to meet community needs, Gale said. “Extending the life of N95 masks was something we wanted to do, so we started work on a solution before we’d secured funding.”
The design was developed by a team consisting of Sergio Solares, technology access manager, Richard Berman, education lead, Joe Brady, a former mechanical engineering student at Camosun who has done the majority of fabricating on the UVen, and Cody Short, a first-year mechanical engineering student, Gale said.
Burman said UV light is a germicide that will kill viruses and bacteria. Inside the device is a reflective surface, where UV light bounces around, he said. “We’ve worked to ensure that all parts of the mask being sterilized inside receive a consistent and strong enough dose to kill the virus.”
Camosun Innovates, based at the Babcock Canada Interaction Lab at the Saanich campus, is making designs freely available so manufacturers around the globe can make their own, which is what it did with its face-shield design.
Western Edison Manufacturing on the Saanich Peninsula is producing the first five prototypes and more are expected in coming months.
Gale said the UVen could also be used in rural and remote communities, as well as other countries where resources are scarce.
“I think this could be really important to the world community and their ability to address [PPE] shortages going forward.”
Canada’s Natural Science and Engineering Research Council has contributed $75,000 toward five models to create prototypes and to test and manufacture them in partnership with Western Edison and Island Health.
Camosun worked with AP Plastics locally on the face shields and is partnering again with that company to use injection molding with the aim of extruding an entire face shield in one process, Gale said.
If the process works well, it might be able to reduce the costs of face shields by 75 per cent and increase the manufacturing speed “astronomically,” he said. That project has also received a $75,000 grant from the federal research council.
The centre has also been working with Island Health on designing a new intubation box, still in the design stage. The plastic shield surrounds patients who have respiratory failure and need a tube inserted into their airway to allow them to breathe.
The intubation process can cause spread of the virus through the air, which has prompted some hospitals to use a type of box, which can be cumbersome and difficult to work with, Gale said.
“We’ve got a team that is redesigning those intubation boxes to hopefully make it more effective for doctors to help patients.”